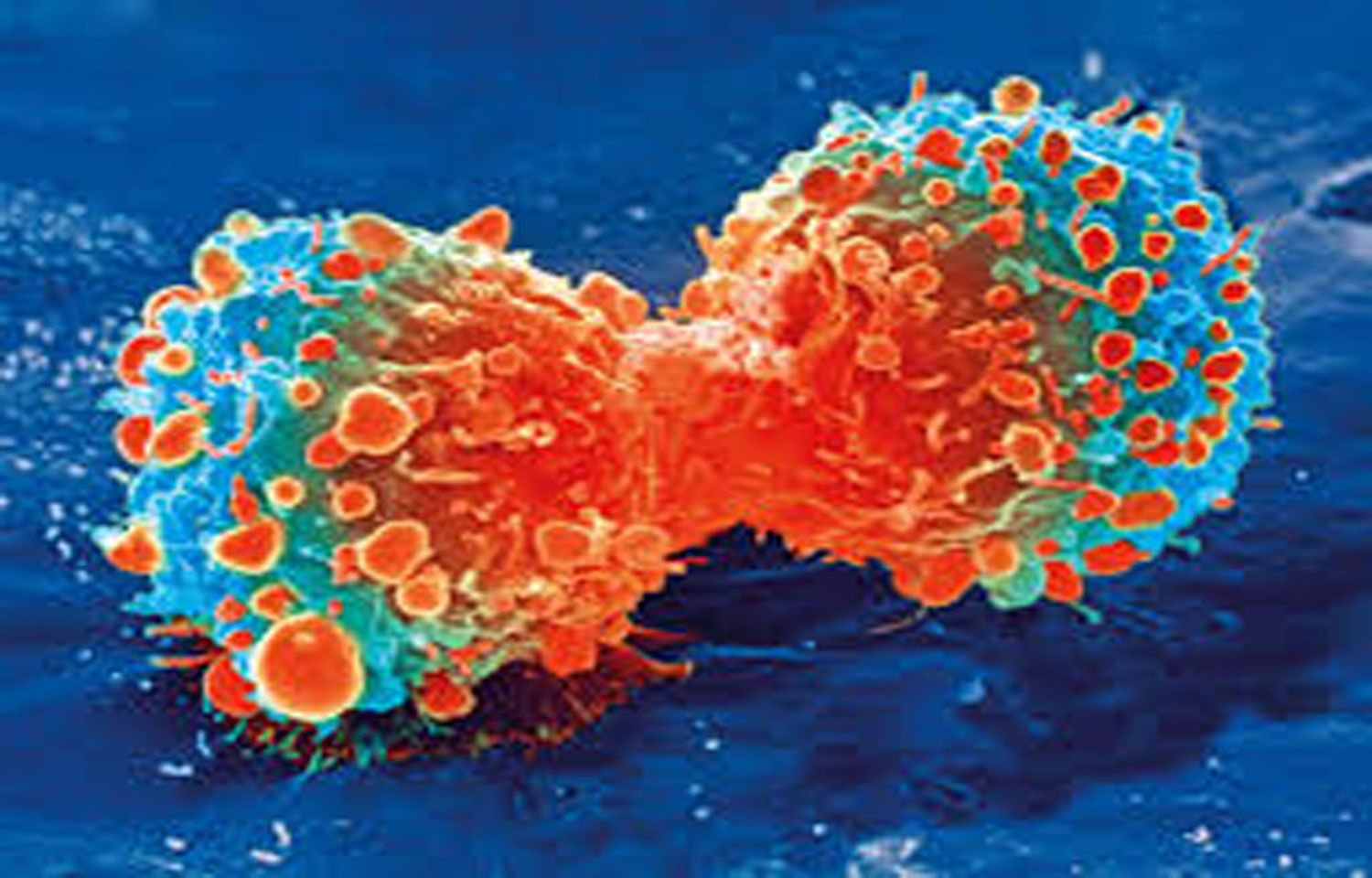
The University of East Anglia is one step closer to developing a new generation of light-activated cancer treatments. The procedure, which sounds futuristic, would work by activating biotherapeutic chemicals by turning on embedded LED lights near a tumour. These new treatments would be far more precise and efficient than the most advanced cancer immunotherapies currently available.
The science underlying this novel concept has recently been revealed by new research. It demonstrates how the UEA team created antibody fragments that not only ‘fuse’ with their target but are also light activated.
It means that immunotherapy treatments in the future may be engineered to target tumours more precisely than ever before.
The principal scientist for this study, Dr Amit Sachdeva, from UEA’s School of Chemistry, said: “Current cancer treatments like chemotherapy kill cancer cells, but they can also damage healthy cells in your body such as blood and skin cells. “This means that they can cause side effects including hair loss, feeling tired and sick, and they also put patients at increased risk of picking up infections.
“There has therefore been a very big drive to create new treatments that are more targeted and don’t have these unwanted side-effects. “Several antibodies and antibody fragments have already been developed to treat cancer. These antibodies are much more selective than the cytotoxic drugs used in chemotherapy, but they can still cause severe side effects, as antibody targets are also present on healthy cells.”
The UEA team has now created one of the first antibody fragments that binds to and forms a covalent bond with its target when exposed to a specific wavelength of UV light.
Dr Sachdeva said: “A covalent bond is a bit like melting two pieces of plastic and fusing them together. It means that drug molecules could, for example, be permanently fixed to a tumour.”
“We hope that our work will lead to the development of a new class of highly targeted light-responsive biotherapeutics. This would mean that antibodies could be activated at the site of a tumour and covalently stick to their target upon light activation.”
“In other words, you could activate antibodies to attack tumour cells by shining light – either directly onto the skin, in the case of skin cancer, or using small LED lights that could be implanted at the site of a tumour inside the body.”
“This would allow cancer treatment to be more efficient and targeted because it means that only molecules in the vicinity of the tumour would be activated, and it wouldn’t affect other cells.”
“This would potentially reduce side effects for patients, and also improve antibody residence time in the body.”
“It would work for cancers like skin cancer, or where there is a solid tumour – but not for blood cancers like leukaemia.”
“Development of these antibody fragments would not have been possible without pioneering work from several other research groups across the globe who developed and optimised methods for site-specific incorporation of non-natural amino acids into proteins expressed in live cells.”
“We employed some of these methods to site-specifically install unique light-sensitive amino acids into antibody fragments.” If the researchers’ next steps are successful, they hope to see the next generation of light-activated immunotherapies used to treat cancer patients within the next five to ten years.