According to a recent study, genetic alterations in Barrett’s oesophagus (BE) cells are an indicator of oesophageal cancer that can be discovered several years before cancer arises.
A team of researchers from the Fred Hutchinson Cancer Research Center reported their findings in the journal “Nature Communications.” The study demonstrates the typical abnormalities, which include big sections of DNA being rearranged and damage to both copies of a tumor-suppressing gene called TP53.
The majority of patients who advanced [to oesophageal cancer] had two “hits” [changes that likely inactivate normal gene activity] on TP53, stated Dr. Thomas Paulson, a senior staff scientist in the Grady Lab who co-led the investigation.
“When compared to patients who did not advance to cancer, cells with mutated TP53 migrated to bigger parts of the oesophagus and remained for lengthy periods of time.”
Though the team’s ultimate objective is to enhance oesophageal cancer diagnosis and screening, Paulson stressed that this study contrasts the mutations and DNA alterations that happened in individuals who progressed to cancer with those that occurred in people with stable, benign BE.
While the findings are important and based on an examination of over 400 tissue samples, he believes that the findings from this 80-patient research would need to be verified in other patient groups before they could be used therapeutically to predict whether additional BE patients may develop cancer.
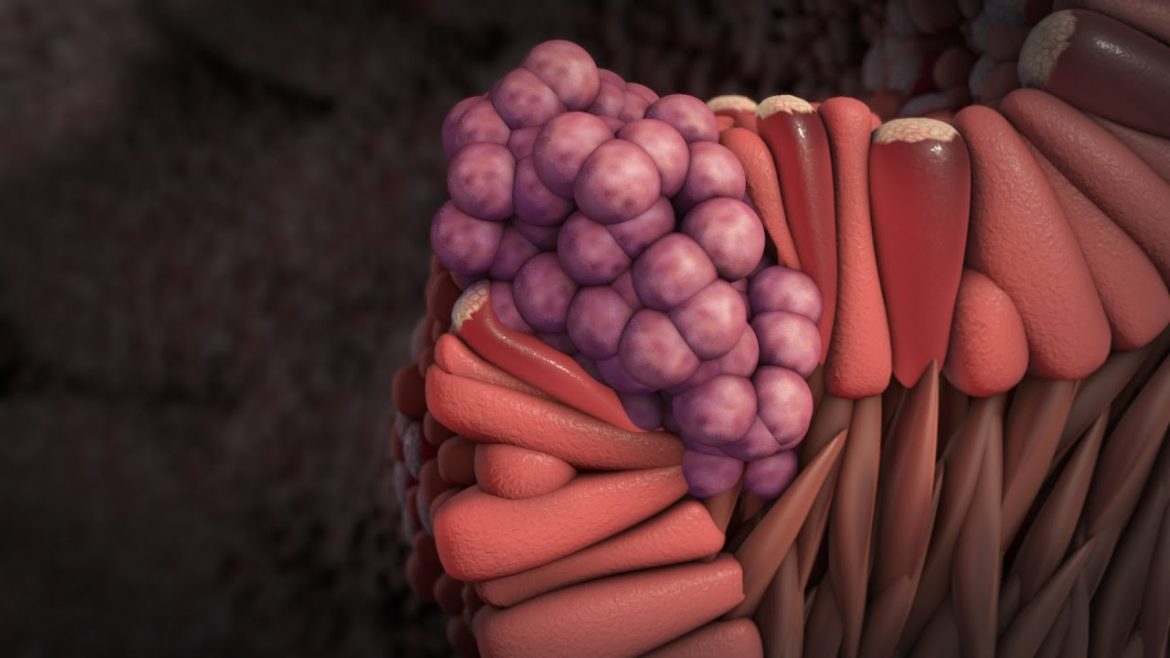
Barrett’s oesophagus develops in certain people who have long-term acid reflux as a new form of oesophageal lining that is more resistant to the harm produced by reflux. Despite the fact that BE is frequently accompanied by DNA abnormalities, the majority of people will never require treatment for their BE, which will stay benign and stable.
Approximately 5% of BE patients may develop esophageal adenocarcinoma, a kind of cancer. Though esophageal cancer is uncommon (approximately 20,000 new cases are discovered each year in the United States), it is deadly; about 20% of patients survive five years after diagnosis.
Once you have advanced esophageal cancer, your therapy choices are extremely restricted, “Paulson explained.
“The therapy possibilities are significantly better if you can identify the tumour while it’s extremely small, even microscopic.”
However, 95% of BE sufferers will never get cancer. Invasive screening and preventative procedures expose individuals to hazards while providing no advantages.
To address this, Hutch’s researchers established the Seattle Barrett’s Esophagus Study in the early 1980s to learn more about BE and how it advances, as well as to identify any genetic markers that indicate people at high or low risk of developing cancer.
The capacity to categorise patients into risk groups, also known as risk stratification, would allow clinicians to provide patients with the appropriate level of screening and intervention.
Because the team has been studying patients for years, they have a lengthy runway to search for hints before cancer takes launch. Previous research on the genetics of BE and esophageal cancer concentrated on alterations to individual genes, but technological breakthroughs now allow scientists to study DNA changes that occur outside of genes (where most of our DNA lies). To find out more, the BE team performed sequencing research on 427 tissue samples that covered all of the DNA in a cell (known as the genome).
The researchers looked at both minor modifications that changed only a few letters of DNA and huge changes that added, erased, or relocated enormous swathes of DNA.First, they discovered that all BE is associated with a large number of mutations, regardless of whether a patient develops cancer or not.
One of the critical results was how many genes that people think of as cancer-driver genes were altered in patients who will never go on to get cancer, said project co-lead Patty Galipeau, a public health sciences research programme manager now in Dr. Gavin Ha’s lab who helped shepherd the years-long project to completion.
One cancer-associated gene, in particular, TP53, stood out in the researchers’ analysis. It encodes a protein that regulates a variety of critical cellular activities, including identifying damaged DNA, repairing it, and promoting cell proliferation.
It’s one of the most frequently mutated genes in all types of cancer, but the researchers discovered that some BE patients who didn’t get cancer also had a TP53 mutation.
However, a closer dig into BE DNA found that the notion that any TP53 mutation causes cancer is oversimplified. Each gene is duplicated in humans (one from each parent). An individual can have a mutation in only one copy (one “hit”) or mutations in both copies (two “hits”) (two hits).
“The majority of progressors had two hits in TP53,” Paulson stated. A person with two hits is at a very high probability of advancing from BE to cancer, but a person with one hit may also advance, he added.
Patients that developed cancer exhibited TP53 mutations in wider sections of tissue compared to non-progressing patients who had single-hit, localised lesions.
It is extremely difficult for a person’s cells to repair damaged DNA if both copies of TP53 are disrupted. This results in enormous portions of DNA being duplicated, deleted, or reshuffled. In fact, the researchers discovered that BE cells from individuals who had oesophageal cancer were considerably more likely to possess these big, complicated alterations than cells from people who did not get the disease.
Even though the current findings aren’t enough to change diagnostic strategies for patients, the work contains important insights that researchers who want to develop a biomarker test should keep in mind, such as the fact that single TP53 mutations aren’t likely to help distinguish between high-risk and low-risk patients, according to Galipeau.
The research aims to integrate these findings with additional data, including other types of genetic analysis, to build an algorithm that may improve screening periods and identify which BE patients are at risk of getting cancer, led by senior author Dr. Xiaohong Li.
According to Galipeau, a brighter future for BE sufferers will rely not only on genetic analysis but also on emerging technologies that make biopsies easy or perhaps unnecessary.
With Ha, Paulson, and the rest of the team, they are looking at the idea of establishing a screening test based on DNA released into the blood from BE cells that indicates a high risk of cancer and ends up circulating in the blood.
A test like this would allow doctors to examine patients’ health in a less intrusive manner, using a blood sample rather than a scope down the throat.
The team also expects that their discoveries will help other cancer researchers. They believe that the genetic modifications they discovered may shed light on how cells adapt to deal with stressful environments—and how those coping strategies might backfire—and that their findings may extend beyond oesophageal-specific cancer pathways.